‘What forms does care take? What does taking care of oneself, another, or each other look and feel like?’ Members of the Waiting Times team recently joined scholars from critical medical humanities, disability studies, the environmental humanities, literary studies and feminist theory in response to the call to think about form as ‘that which might productively organise but also capture the protean nature of care’. These books, articles and projects are a selection of the work engaged in presentations and discussions across the workshop. They are shared here as a resource for others and to mark the event which took place online on the 9th and 10th September. The forms of care workshop was organised by Dr Erin Lafford (Oxford) and Dr Alexandra Kingston-Reese (York) courtesy of the University of York.
Details of individual presentations can be found below the reading list.
Forms for care conference – reading list selection:
Burke, L. (2014). Oneself as another: Intersubjectivity and ethics in Alzheimer’s illness narratives. Narrative Inquiry, 4(2), 28-47.
Butler, J. (2021) The Force of Nonviolence: An Ethico-Political Bind. Verso.
Fuchs, E (2005) Making an Exit: A Mother-Daughter Drama with Alzeheimer’s, Machine Tools, and Laughter. Metropolitan: New York.
Harney, Stefano, and Fred Moten. The Undercommons: Fugitive Planning & Black Study (2013) New York: Minor Compositions
Hedva, Johanna. (2015) ‘My Body Is a Prison of Pain so I Want to Leave It Like a Mystic But I Also Love It & Want It to Matter Politically.’ Lecture, Human Resources, Los Angeles, October 7.
Jacoby, O. (1919/2019) Words in Pain: Letters on Life and Death. Ed. by J. Catty and T. Moore. Oxford: Skyscraper Publications.
Karjevsky G., Talevi, R., Bailer, S., (eds) (2020) Letters to Joan Tronto. With Edna Bonhomme, Johanna Bruckner, Teresa Dillon, Joao Florencio, Johanna Hedva, Elke Krasny, Patricia reed, Yayra Sumah and Joan Tronto. New Alphabet School.
Kittay, E. F. (2003) The Subject of Care: Feminist Perspectives on Dependency (Feminist Constructions). Rowman & Littlefield Publishers.
Stengers, I., (2011) The Care of the Possible: Isabelle Stengers interviewed by Erik Bordeleau, Landscape, Architecture, Political Economy, (1): 12-17.
Schaffer, Talia (2021) Communities of Care: The Social Ethics of Victorian Fiction. Princeton, N.J.: Princeton University Press.
The Care Collective (2020) Andreas Chatzidakis, Jamie Hakim, Jo Littler, Catherine Rottenberg, and Lynne Segal. The Care Manifesto: the Politics of Interdependence. London: Verso.
The Mind’s Eye (2021) Care Syllabus. MCLA. https://www.caresyllabus.org/about
Mol, Annemarie, Ingunn Moser, and Jeannette Pols (2010) ‘Care: Putting Practice into Theory’, in Care in Practice: On Tinkering in Clinics, Homes and Farms, ed. by Annemarie Mol, Ingunn Moser, and Jeannette Pols (Verlag, Bielefeld: transcript).
Out of the Woods Collective (2020) Hope Against Hope: Writings on Ecological Crisis. Brooklyn, NY: Common Notions.
Whitehead, Anne. (2017) Medicine and Empathy in Contemporary British Fiction: An Intervention in Medical Humanities. Edinburgh: Edinburgh University Press.
Programme:
Elizabeth Barry, ‘We Hang Up Laughing: Dementia, Care and the Temporality of Laughter’
Marie Allitt, ‘Stratifying Care: Geology and Grammar of Cancer and Hospital Care in Peter Reading’s C’
Lucy Burke, ‘Taking time: Reading Ali Smith’s There But For I as a form of care’
Alice Hall, ‘Caring and Curating: Women, Work and the Carers UK Archive’
Zoe Weinberg, Jade Colon, Amira F. Hassan, and Savanna Schaefer, ‘The Free Form of Freewriting as a Form of Care’
Elisabeth Pedersen, ‘The Catholic Worker Care Model: Building Interdependent Caring Communities and Kinships’
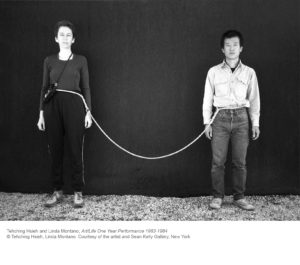
Lisa Baraitser and Stephanie Davies, ‘Waiting as Care’s Form: Notes from the Waiting Times Project’
Michael Flexer, ‘Signs You Care: Form in the Semiotic of Caring’
Jocelyn Catty and Laura Sailsbury, ‘Writing into the Future: Letters as Containers of Time and Care’
Jordan Osserman, ‘The ‘Object’ of the Puberty Blocker’
Kelechi Anucha, ‘Form and Fugitive Care’
Nicola Kirkby, ‘Care and Repair: Narrative Infrastructure in Elizabeth Gaskell’s Ruth (1853)’
David James, ‘Pathographic Close Reading’
Levi Prombaum, ‘A No Manifesto for Caring in Cultural Interpretation’
Victoria Papa, ‘Caremaking: Beyond Give & Take’
Laura Thompson, ‘Museological Critiques and Accessibility’
Stephanie Davies