MAKING THE MOST OF WAITING
Notes from the Waiting Time workshop held at the Wellcome Centre for Cultures and Environments of Health, 12 June 2019
If time is a great healer, is waiting the problem?
Florence Nightingale (1859) certainly thought so. She saw it as bad for health – “apprehension, uncertainty, waiting (my italics), fear of surprise…do a patient more harm than any exertion.” It’s tiresome too, as the Kinks noted in 1965 and in the meantime, we’re all Waiting for Godot (who never comes). For health systems, waiting is a mark of inefficiency that undermines ‘customer’ confidence. It is a focus for targets and management expedients in a culture which expects action, now!
But, is this the whole story?
Earlier this summer, a workshop at Exeter showed that – sometimes – embracing the wait can be its own reward. It’s the quality of care and use of the time spent waiting that makes the difference between a ‘good’ and a ‘bad’ wait. It was a reminder that, sometimes, ‘wait and see’ is a plausible alternative to immediate action when treatments and outcomes are uncertain.
A long wait can allow health issues to resolve through natural healing. Rest and recovery may produce a better outcome than immediate surgery. But, waiting can also mean delay, with later diagnosis and treatment and even earlier death if serious conditions are not caught in time. The challenge – as ever – is to determine priorities from among competing needs. For example, handlers seeking to make the right call on waits for ambulances face an acute dilemma balancing availability of transport with urgency, system rules and patient need.
Waiting allows for exploration and for time to assess progress. ‘Watchful waiting’ at gender identify clinics allow young people to grow while services explore and assess their development. Such exploration can, however, mean suffering for young people clear in their desire to transition, not least by allowing the physical developments that will make the eventual transition harder. Parents and carers are not always persuadable about the merits of such delay and may be suspicious of delays in accessing scarce services. The right words can help. ‘Active monitoring’ seems to work better than ‘watchful waiting’.
Waiting – not always so bad?
Waiting can also support the therapeutic process. It can validate individual experience as the end of life approaches, affirming the value of lives lived for individuals and their families. Creative expression and appreciation through poetry, music, painting (van Gogh’s “Starry Night” was given as a stunning example) and nature can provide a vehicle for this approach. Importantly, it reminds people that they are not just “boring old farts”, as one participant in the Waiting Times’ hospice project remarked.
The policy challenge is to acknowledge – and balance – the positive aspects of waiting with the negative aspects of delay in care and treatment. This challenge will be met by better understanding the social and cultural context of such care, by harnessing patient experience – including meeting concerns about being fobbed off because of a lack of – or cuts in – available services, and reflecting these concerns in the design and delivery of services that are welcoming and available to all.
Developing services that reflect the positive aspects of waiting will require:
- changing the character of public services by putting the individual at the heart of service provision, and through greater transparency and dialogue about the options for care and treatment;
- being straight about the role that access to services – or lack of it – plays in creating harmful delays and widening health inequalities; and
- restoring the care and support of individuals to a central place in the work and training of professionals, and allowing sufficient time in day-to-day routines to ensure a good quality of care.
This will not be easy.
The Centre’s DeStress project has shown how stigma and deterrence have re-entered the public service lexicon affecting its character, and citizens’ experience. Vulnerable and disadvantaged people bruised by claiming welfare benefits fear this ‘hostile environment’ will seep into the health service, notwithstanding the efforts of the NHS to resist it. It can take time to build courage to visit the GP and while waiting at the surgery, people feel anxious, doubtful they should be there, and guilty about wasting the doctor’s time when services are under strain. This is a recipe for an unsatisfying consultation. A rapid reach for the prescription pad can only reinforce patient doubts and wider sense of powerlessness, which – in turn – acts as a barrier to further engagement and greater risk of ill-health
Timely access to services will help maintain good health and prevent disease but this is difficult to achieve with big differences in service provision – and waiting times – across the country. The ‘inverse care law’ – where the availability of good medical or social care tends to vary inversely with the needs of the population served – is alive and well.
While there is no ‘one size fits all’ formula for waiting – patient need and the training and capacity of professionals vary – the workshop heard that professionals holding hands across a ‘shark infested sea of uncertainty, diagnosis and treatment to an island of recovery or resolution’ can maintain the dignity, mental health and wellbeing of individual patients during this journey. Yet, social workers and others are not always able to sustain this caring role, given today’s emphasis on management organisation and cost concerns. Volunteers often have to fill the gap. There is a poor fit too between family needs and the organisation of primary care, and a lack of clarity about available support services.
“Don’t forget,” said Florence, “patients are shy of asking,” and without explanations they remain in ignorance about why they are waiting. A situation where ‘nothing happens, nobody comes and nobody goes’ is disorientating. It also reflects professional uncertainty and a lack of confidence in the system. Everyone wants health services that are delivered in a fair, timely and appropriate way. However, better waiting list management will not deliver this on its own without a clear focus on the quality and time taken over the care and treatment of individual patients, and the views and experiences of patients themselves.
This blog was written by Dr Ray Earwicker, honorary fellow, Wellcome Centre for Cultures and Environments of Health, University of Exeter






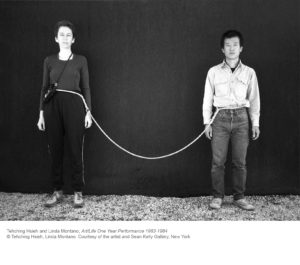
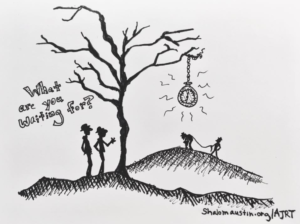 Some things emerged that we’re still thinking through together. First, what does care have to do with ‘thirdness’? This term emerges from relational psychoanalysis to try to describe the way that care doesn’t flow simply from one to another, but is mediated by a third term (or the co-creation of a third relational entity) that takes us beyond the ‘doer and done to’ dynamics that Jessica Benjamin identified in The Bonds of Love. Raluca talked of how the psychoanalytic encounter creates something new which we don’t own, and we can’t fully control, that exists beyond the two but is used actively in the therapy, and constitutes acts of recognition and witnessing. Psychoanalytic care involves a systematic technical effort to hold yourself across different threads of time – a kind of ‘doing time’ in which time is always a verb. The presence of these multiple threads in the same moment of the analytic session is particular to psychoanalytic work. Waiting, from this perspective is less about waiting for, and more about waiting with, which Laura identifies as a key modernist temporality (think of Samuel Beckett’s Waiting for Godot). Raluca’s work, in particular, argues that the Budapest school of psychoanalysis offers a way to understand ‘a true third’ that is the work of analogy (one set of relations has a relation to another set of relations, and this creates something else, a third set of relations). This idea of thirdness could relate, however, to institutions where care takes place, such as the NHS, or the art gallery, that also mediate relations of thirdness that could be thought about as practices of care. Deborah, in particular, took up this idea of the art gallery or space as a third space where care can circulate.
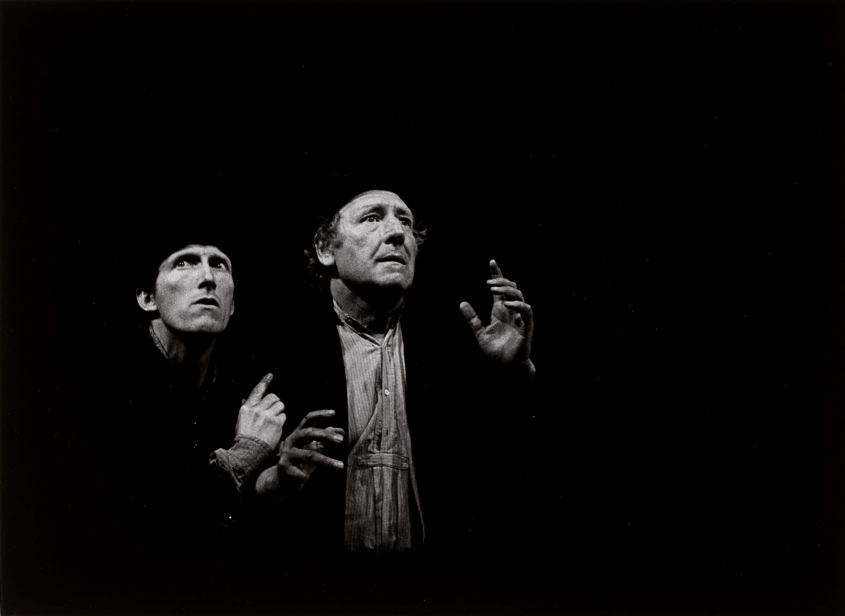
Some things emerged that we’re still thinking through together. First, what does care have to do with ‘thirdness’? This term emerges from relational psychoanalysis to try to describe the way that care doesn’t flow simply from one to another, but is mediated by a third term (or the co-creation of a third relational entity) that takes us beyond the ‘doer and done to’ dynamics that Jessica Benjamin identified in The Bonds of Love. Raluca talked of how the psychoanalytic encounter creates something new which we don’t own, and we can’t fully control, that exists beyond the two but is used actively in the therapy, and constitutes acts of recognition and witnessing. Psychoanalytic care involves a systematic technical effort to hold yourself across different threads of time – a kind of ‘doing time’ in which time is always a verb. The presence of these multiple threads in the same moment of the analytic session is particular to psychoanalytic work. Waiting, from this perspective is less about waiting for, and more about waiting with, which Laura identifies as a key modernist temporality (think of Samuel Beckett’s Waiting for Godot). Raluca’s work, in particular, argues that the Budapest school of psychoanalysis offers a way to understand ‘a true third’ that is the work of analogy (one set of relations has a relation to another set of relations, and this creates something else, a third set of relations). This idea of thirdness could relate, however, to institutions where care takes place, such as the NHS, or the art gallery, that also mediate relations of thirdness that could be thought about as practices of care. Deborah, in particular, took up this idea of the art gallery or space as a third space where care can circulate. Secondly, we thought through questions of mourning and lamentation that are embedded in the etymology of the term ‘cara’ (trouble, grief, sickness, think of ‘what is this life, if full of care’, from William Henry Davies’s poem ‘Leisure’, where care means difficulty). We thought together about how difficult it is to describe the quality of time as we feel it in the body, and the way that the granular surface of the symptom – depression for instance – has to be observed, described and looked at in a phenomenological way. Our engagement with Eugene Minkowski’s early phenomenological psychiatry offers a way to do this. But lamentations also came up around the
Secondly, we thought through questions of mourning and lamentation that are embedded in the etymology of the term ‘cara’ (trouble, grief, sickness, think of ‘what is this life, if full of care’, from William Henry Davies’s poem ‘Leisure’, where care means difficulty). We thought together about how difficult it is to describe the quality of time as we feel it in the body, and the way that the granular surface of the symptom – depression for instance – has to be observed, described and looked at in a phenomenological way. Our engagement with Eugene Minkowski’s early phenomenological psychiatry offers a way to do this. But lamentations also came up around the 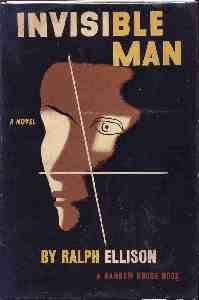 Finally, we thought about the giving of time as a form of taking care of the other that can’t be read in a straight forward way. Deborah talked about those who are ill and those who offer care and the ways that these interactions become the source of an artwork. Visual imagery and sound contain the intimacy of those conversations, raising questions about how to care for those images. Her work involves ‘thinking in darkness’ – working literally in the dark to select fames of film and then re-film them, using material from one temporal realm and transferring it to another (the gallery). Is there an aesthetics, then, of care, and can it take place in the gallery? Wilfred Bion talks about psychoanalytic attention as a ‘beam of darkness, a reciprocal of the searchlight’, which inverts the idea of thinking shining light on darkness. How rather does darkness, as a beam, intervene in light, and in what sense is this a careful practice? Thinking with Ellison’s Invisible Man, invisibility, after all, gives you a slightly different sense of time, of being behind the beat or in front of it, but not ‘in time’. Elizabeth Freeman’s notion of the deviant pause of sexual practices within the normative community does the same work here. In her presentation later in the symposium, Laura also noted how the slow reading the ‘perverse’ rhythms of Beckett’s prose work seem to demand elicits forms of attention, which are potentially careful, to the weight of the world. Such practices produce care as a different or queer way of thinking, or making sense, without sense appearing as prior to knowledge. We are always disrupted, after all, by the time of the other.
Finally, we thought about the giving of time as a form of taking care of the other that can’t be read in a straight forward way. Deborah talked about those who are ill and those who offer care and the ways that these interactions become the source of an artwork. Visual imagery and sound contain the intimacy of those conversations, raising questions about how to care for those images. Her work involves ‘thinking in darkness’ – working literally in the dark to select fames of film and then re-film them, using material from one temporal realm and transferring it to another (the gallery). Is there an aesthetics, then, of care, and can it take place in the gallery? Wilfred Bion talks about psychoanalytic attention as a ‘beam of darkness, a reciprocal of the searchlight’, which inverts the idea of thinking shining light on darkness. How rather does darkness, as a beam, intervene in light, and in what sense is this a careful practice? Thinking with Ellison’s Invisible Man, invisibility, after all, gives you a slightly different sense of time, of being behind the beat or in front of it, but not ‘in time’. Elizabeth Freeman’s notion of the deviant pause of sexual practices within the normative community does the same work here. In her presentation later in the symposium, Laura also noted how the slow reading the ‘perverse’ rhythms of Beckett’s prose work seem to demand elicits forms of attention, which are potentially careful, to the weight of the world. Such practices produce care as a different or queer way of thinking, or making sense, without sense appearing as prior to knowledge. We are always disrupted, after all, by the time of the other.